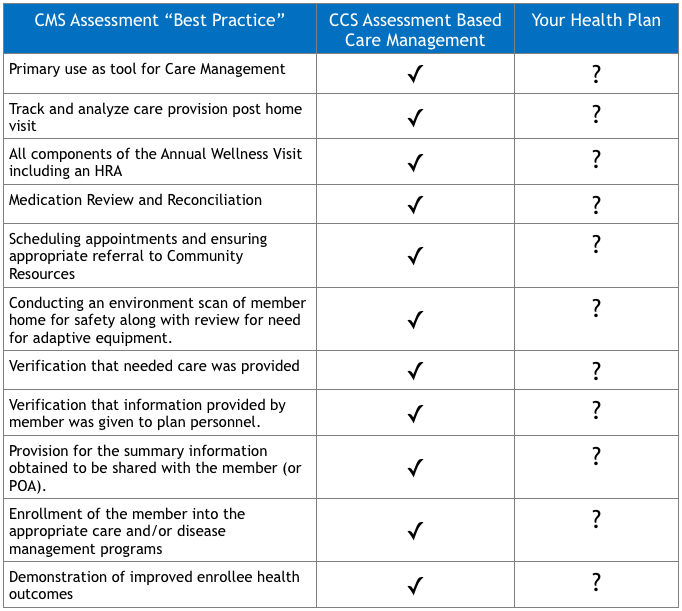
The CMS Best Practices and expectations as evidenced in the “Draft Call Letter” is to utilize Home Assessments to influence Beneficiary Care Plans. ComplexCare Solutions has managed face-to-face in-home assessments to align with care plans as a standard practice, and our model influences beneficiary care and coding accuracy.
Executive Summary:
ComplexCare Solutions, Inc. (CCS) is pleased with CMS’ affirmation of the clinical value of in-home assessments and its promulgation of “Best Practices” recommendations. CMS’ “Best Practices” align with CCS’ current process that connects the in-home face-to-face assessment to high touch, high value care management. CCS has always used the in-home face-to-face assessment as an opportunity to develop NCQA compliant care plans and utilize care management services to reduce cost and improve health outcomes. CCS has always been ahead of the curve and has built our tools and processes to exceed CMS’ best practices guidelines by linking assessments to care management. It never made sense to assess members in their home, build a relationship and come away with diagnoses and information only for the purposes of risk adjustment. Our solutions are built around the principle that data driven tools like assessments play an integral role in engagement of members and development and execution of care plans.
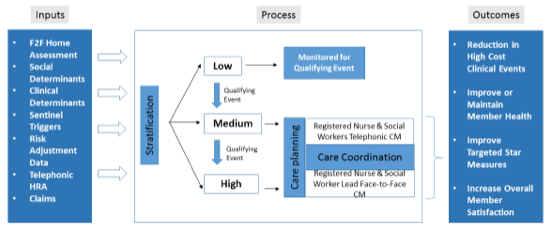
CCS creates the link between face-to-face assessments and quality care management. Our member engagement strategies use a combination of proprietary algorithms to analyze claims data, clinical, socioeconomic, behavioral and environmental information to identify impactable members who have both the will and the need to benefit from home-based interventions. Our modular suite of services is designed to integrate with your operations at any or all points of care to form a customized solution. In every case, we provide ongoing analysis and reporting to measure program performance, while ensuring strict compliance with CMS, State and NCQA regulations.
CCS’ program exceeds CMS’ best practice recommendations for in-home assessments while delivering a 6:1 ROI as part of our integrated Care Management suite of services.
We combine those elements to properly stratify a member population into disease agnostic severity levels that identify impactable members that will benefit from a broad array of care management strategies. Placing these individual members into the right care management approach is the clear differentiators in health outcomes and client/member satisfaction levels. We then are able to leverage the strong bond and relationship we have developed with the member to drive adherence to care plans and healthy outcomes. We bring value to the member, the plan and the provider by reducing medical cost trend, improving quality Star measures, escalating members to care management and improving member satisfaction.
It is important that health plans are aligned with CMS’ best practices to avoid Compliance Actions or Civil Monetary Penalties. CCS has always been built to maximize the quality of care and not to maximize the amount of unnecessary diagnoses. CCS believes it is important to have a strong compliance organization and our orientation is based on enhancing the member’s quality of care.
There are now implications for 2016, and the industry may see a drop in member risk scores and associated revenue. CCS is again ahead of the curve and we have the tools to drive care plans for beneficiaries while also managing accurate coding and compliant standards and protocols.
CMS’ Best Practices for In-home Assessments:
CMS outlined best practices after receiving input from over 100 plans. When deployed, these best practices provide measurable impact on plan performance and service quality. CCS has engaged and submitted comments to CMS promulgating the necessity to use the data captured during a face-to-face in-home assessment for effective care management.
CCS has always been a care management company and our current services are already aligned with CMS’ best practices. Since the beginning our assessments were built to improve the quality of care and serve as a link to care management. We have proven that our in-home assessments and high touch, high value care management are an effective solution to keep your at-risk members in their homes and community. CCS wants to talk to you about how we can develop joint solutions utilizing our established and customizable workflows, tools and care management practices to make sure your members are satisfied and get the care they need.
The ComplexCare Solutions Advantage:
ComplexCare Solutions excels at delivering face-to-face in-home assessment and high-touch, high-value care management services for health plans nationwide. We are known for our successful in-home member engagement, which allows us to collect a more robust range of data, implement more personalized care plans and motivate change for desired outcomes. Our modular suite of specialized services is designed to integrate with your operations across the entire care management continuum to build a customized solution that helps you stay in compliance, receive appropriate reimbursements, lower costs and improve member satisfaction.
Our executive team, clinicians and coders, bring a wealth of experience and dedication to our shared goal of delivering the best care management solutions in the industry. With decades of working with health plans large and small, we bring a deep understanding of your business challenges to every engagement, and firm resolve to helping you achieve your goals. We currently contract with three of the five largest national health plans as well as many regional, local and special needs plans. The vast majority of the members we serve are Medicare Advantage and Dual-Eligibles. We also serve Managed Medicaid, Commercial ACA and General Commercial Populations. We are ACAP-endorsed and we provide assessment and care management services across the U.S. and Puerto Rico, with an average daily care management census of over 12,000 members. In 2015, we expect to complete over 200,000 high-touch, face-to-face member engagements.